Turn any unstructured file—claim forms, EOBs, physician notes, scanned charts, email attachments—into clean, standardized data in seconds. Advanced OCR, NLP and template driven recognition replace manual chart review while secure, audit ready logs and role based controls maintain HIPAA compliance. Deploy ChartXtractor to cut data capture time by up to 70% and free your staff for higher value work.
Turn any unstructured file—claim forms, EOBs, physician notes, scanned charts, email attachments—into clean, standardized data in seconds. Advanced OCR, NLP and template driven recognition replace manual chart review while secure, audit ready logs and role based controls maintain HIPAA compliance. Deploy ChartXtractor to cut data capture time by up to 70% and free your staff for higher value work.

Automate your entire claims cycle—from status checks and ERA processing to payment posting, appeals and reconciliation. ClaimXpert’s business‑rules engine and intelligent CARC/RARC extraction drive faster reimbursements and boost first‑pass yields, while encrypted audit trails ensure full compliance. Scale AR operations without adding headcount and reduce operating costs by up to 40%.

Eliminate eligibility and prior‑authorization delays at the front desk. TrustVerify logs into multiple payer portals and APIs to pull real‑time coverage details—copays, deductibles, coinsurance—and tracks authorization statuses before the patient encounter. Integrate verified data directly into scheduling and billing systems to cut pre‑service denials by up to 25% and speed check‑in, all with audit‑ready logging.

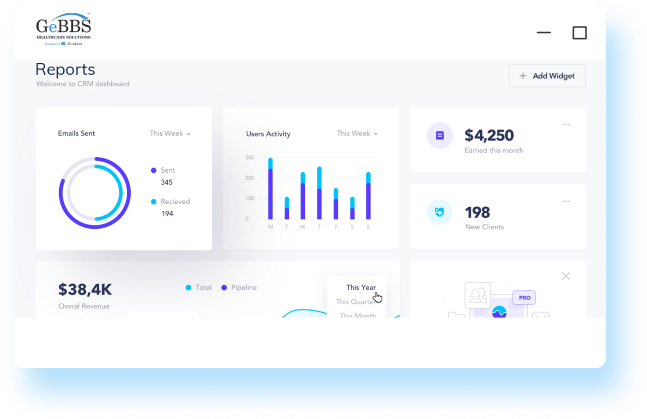
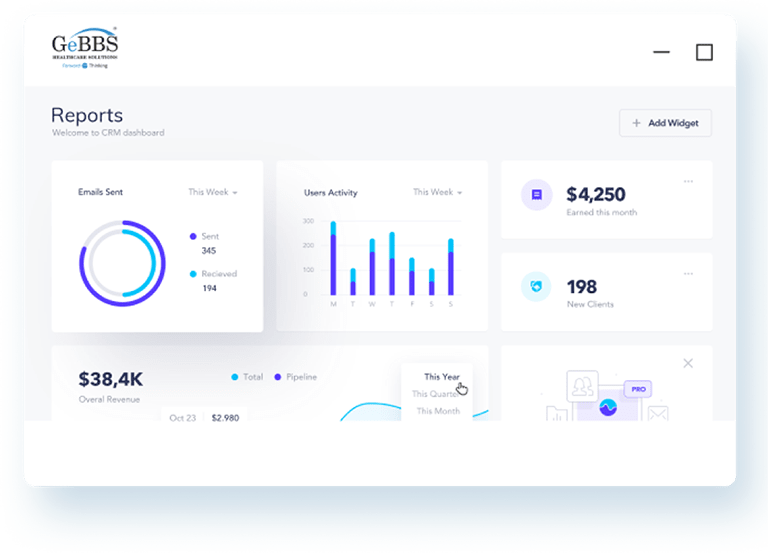
Centralize back‑office task orchestration with rule‑based routing, real‑time dashboards, and desktop tickers. ClaimFlow groups and allocates work items, auto‑generates standardized notes, enforces SLAs, and balances workloads across teams—ensuring consistent quality and up to 20% fewer errors. Keep your revenue cycle on track from initial intake through final resolution.